
The use of Night-time Ventilation for People with SMA
Jennifer Trust Information Leaflet N° 005.Created in conjunction with Anita Simonds MD FRCP,
Royal Brompton Hospital.
 |
The use of Night-time Ventilation for People with SMAJennifer Trust Information Leaflet N° 005.Created in conjunction with Anita Simonds MD FRCP, Royal Brompton Hospital. |
 WHAT IS A BiPAP or CPAP?
WHAT IS A BiPAP or CPAP?
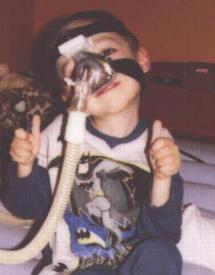
Both are machines used to assist breathing. Usually via a nasal mask. The picture is of a five year old child with type II SMA using a BiPAP.
BiPAP: Bi = two way, PAP= Positive air pressure. Literally translated this means two way positive air pressure. Two-way relates to inhalation (breathing in) & exhalation (breathing out). Therefore a BiPAP is a machine which assists both breathing in and out.
CPAP: C= Constant, PAP= Positive air pressure. Therefore CPAP = Constant positive air pressure. Used to maintain lung expansion and reduce upper airway collapse.
WHY IS VENTILATION USED AT NIGHT-TIME?
A BiPAP/CPAP can be used at any time, however there is a growing argument for its use at night (for people with neuro-muscular conditions) when the respiratory system slows down. SMA affects the respiratory muscles and (which include the diaphragm and intercostal muscles) therefore breathing and respiratory issues can become increasingly problematic for people affected by SMA. This problem is made worse at night when the respiratory system works less effectively and the breathing becomes naturally more shallow. This situation is exacerbated further by the weight of the body when lying down. There is growing concern that impairment of ventilation leads to a build up of carbon dioxide in the bloodstream (hypercania) leading to problems during the day (see below). Left unchecked or treated incorrectly ultimately this can lead to coma or respiratory failure.
WHY NOT JUST USE OXYGEN?
The problem with using oxygen is that it can trick the brain into thinking the respiratory system is working efficiently and can actually make the problems worse. The body is encouraged to breathe even less deeply therefore increasing carbon dioxide levels rather that reducing it.
WHAT ARE THE SIGNS OF CARBON DIOXIDE BUILD UP?
It is impossible to state that any signs definitely point to carbon di-oxide build up, however we have listed some of the possible symptoms:
|
|
|
WHAT DO I DO ABOUT IT?
There are two schools of thought - one is to undergo a full and complete sleep study; this usually involves a stay in hospital and measures bodily function (focussing on respiration) during sleep. The patient is wired to a variety of machines and the movement and respiratory function of the body is stored in a computer to be analysed during the day. One of the important factors for measurement is Carbon Dioxide level.
The other is simpler and it may be possible to borrow the equipment from a hospital to use at home. An oxymeter is attached to the person finger or toe and this measures the oxygen content of the blood throughout the sleep cycle. The results can be stored (for monitoring) on a paper print out. An oxygen saturation level of below 95% requires detailed analysis. In both cases a respiratory specialist would analyse the results and discuss and decide any possible course of action with the individual or the child's parents.
HOW DO I ORGANISE A SLEEP TEST?
Ask your GP, Paediatrician or Neurologist for a referral to a Respiratory Specialist.
IF I NEED A BiPAP/CPAP HOW WILL IT BE FITTED?
A suitably qualified medical practitioner will undertake the fitting of the correct mask. It is important that any mask used for a respiratory device is leak proof and airtight. If the first mask does not fit, don't worry, there are currently more than 15 different types of mask available for BiPAP/CPAP. Some can be customised to the individual.
Below are some comments from individuals who currently use BiPAP/CPAP Machines for night-time ventilation.
An Adult User's opinions:
1/ The BI-pap uses air not oxygen (although it can if needed)- There are no cylinders.A parent of a child user:
2/ Uses Nasal Mask - not a full-face mask - you can still talk and call out without problem. The masks have soft edges and are not uncomfortable.
3/ The whole thing is small, light and easily moved. You can take it anywhere.
4/ It sounds like a hair dryer - not so noisy to disturb sleep.
5/ Exercises lungs - physiotherapy from inside. May stop damp patches settling in lungs and becoming infected.
My main feeling is that when I wake up, I am awake! I feel as if I've had a beneficial nights sleep. I need to be turned much less frequently and have fewer headaches and don't feel so weary and lethargic. It is a totally positive thing with no bad effects at all.
My child had a simple sleep study and was shown to be fine, however it became clear to me this was not the case and I insisted on a trail period using BI-PAP. After much convincing She was provided with one on a trial period and we have never looked back. The results were plain to see within one night's use.Another parent:
It feels like walking into a gale force wind - takes some getting used to. My son is now 4; he has used the BiPap at night regularly since he was 2½ . I am biased I think it is an amazing piece of equipment and have no doubts that without it, he would not be with us now.
© JTSMA, May 2001